Research Updates
By Benjamin Bitler, PhD
Like many cancers, ovarian cancer tumors are composed of many different cell types, including immune cells and cancer cells. There is important information to be learned on how these cells are organized within the tumor, including the potential response to therapy. The complexities of the tumor environment were highlighted by Drs. Clauset, Bitler, and Behbakht in an editorial published in Science Advances. Further, at the University of Colorado Human Immune Monitoring Shared Resource, the Ovarian Cancer Research Group in collaboration with Dr. Julia Wrobel used state of the art technology to examine the organization of ovarian cancer tumors. They found that the spatial relationship of two immune cell types correlated to improved patient outcomes. In July 2021, they published the results of their study in Molecular Cancer Research.
Most patients with a gynecologic malignancy will undergo a surgery at some point in their treatment course. Dr. Carolyn Lefkowits is a leader in the field of palliative care and recently published a medical review on optimal strategies for managing patient’s pain following a surgery. The topics covered in the review include multimodal pain management to reduce post-operative opioid use, pain management in patients with chronic pain and/or history of substance use, and pain management for patients near the end of life. In July 2021, her review was published in Surgical Oncology Clinics of North America.
In today’s cancer clinics, the result of genetic testing provides patient-specific information to the oncologists, which potentially allows for a more individualized treatment plan. Over the course of the last year, Dr. Bradley Corr has been evaluating the genetics of recurrent endometrial cancers. Based on his evaluations, Dr. Corr’s research team defined the risk of recurrence based on a specific genetic mutation. Furthermore, in the lab, he has worked to optimize a novel therapy that is tailored to this specific mutation, and in August 2021, these results were published in Molecular Carcinogenesis.
FAQ*
By Kian Behbakht, MD, MBA
*Please consult with your gynecologists before altering any clinical care.
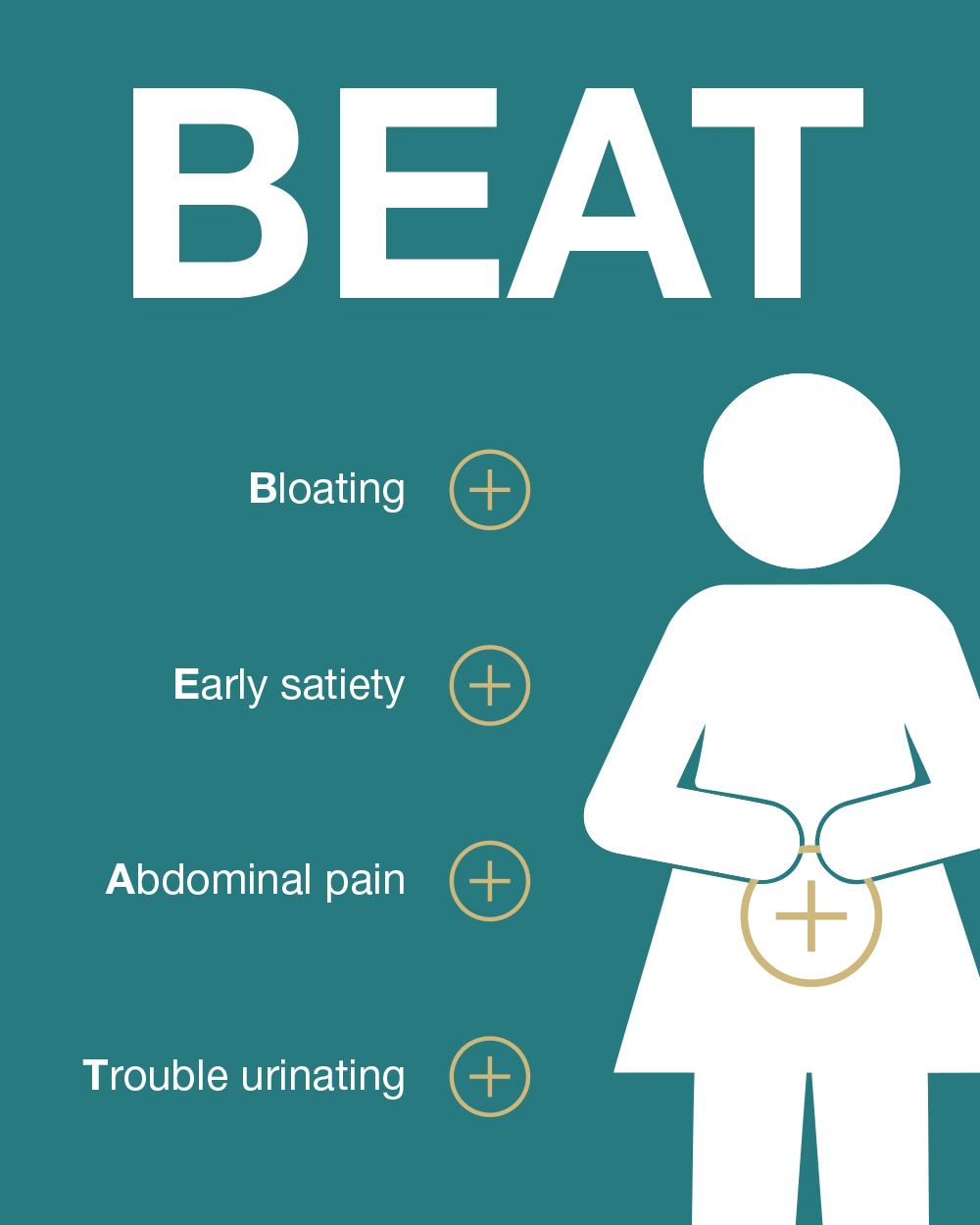
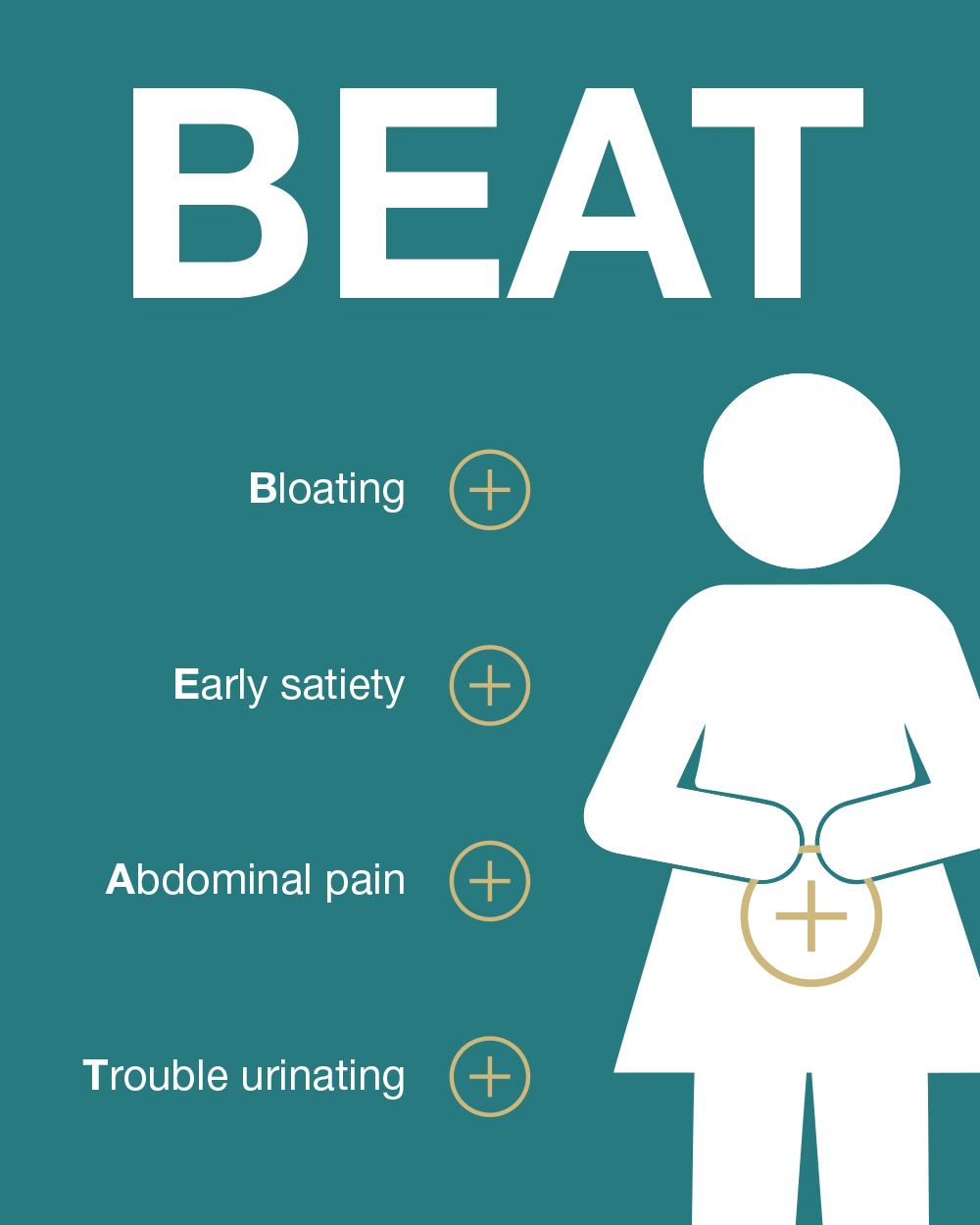
Q: With respect to detecting ovarian cancer early, are there any related symptoms that I should be aware of?
A: The symptoms for ovarian cancer are subtle and are often dismissed as “common.” The symptoms include Bloating, Early satiety, Abdominal pain, and Trouble urinating (BEAT). Based on the National Ovarian Cancer Coalition, if you are experiencing these symptoms for greater than two weeks, please consult your gynecologist. If a cancer is suspected, a gynecologic oncologist should be consulted.
Q: Can I prevent ovarian cancer by having my ovaries removed?
A: The most common type of “ovarian” cancer (high grade serous) is now understood to originate from within the fallopian tubes. In women with a genetic predisposition to breast and ovarian cancers, such as carriers of BRCA1 and BRCA2 mutations, removing the ovaries and fallopian tubes can greatly reduce the risk of ovarian cancer. Hence it is very important to identify families that carry these genetic risks and offer them testing for genetic predisposition (also called cascade testing). In women without genetic risk, the ovaries are important to overall health and should not be removed without clear medical indication.
Q: What is the difference between germline and tumor testing? What is the benefit of germline genetic testing?
A: There are different types of genetic testing. Germline testing refers to assessing genetic markers that are present in every cell in your body. Tumor testing (also referred to as somatic) examines genetic abnormalities present in the tumor cells. Based on the genetic markers, genetic counselors and oncologist have a clearer picture of that individual and family members cancer risk. For additional information on genetic testing please visit the UCHealth genetic testing and counseling website.
Clinical Trial Updates
By Bradley Corr, MD
The Division of Gynecologic Oncology at the University of Colorado has established itself as one of the leading centers in the country for clinical trials. Every year we are recognized as top enrollers to local, national, and international clinical trials. The faculty in our division hold several leadership positions in the national organizations such as the NRG and GOG (Gynecologic Oncology Group). Not only are we often a participating center in the clinical trials, but our providers are also the principal investigators responsible for developing these trials.
The goal of our division is to be able to offer clinical trial opportunities to each of our patients and discuss if it is the right decision for them. We offer a wide range of clinical trials from phase 1 to phase 3, and we often have multiple clinical trial options for each patient. We carry a breadth of trials sponsored by the National Cancer Institute (NCI) and industry, as well as local investigator-initiated trials. We believe trongly that clinical trials should be an option for all our patients.
If you are interested in learning more about clinical trials at The University of Colorado Cancer Center, please visit the Women's Cancer Developmental Therapeutic Program.
New Grant Updates
By Benjamin Bitler, PhD
The ability to conduct cutting edge and innovative research is dependent on grants. In the last six months, faculty in the Division of Gynecologic Oncology and its research partners in the Division of Reproductive Sciences at the University of Colorado have applied to 10 research grants and have been awarded 8 research grants. The grants are funded through a variety of sources including the National Institute of Health, the Department of Defense Ovarian Cancer Research Program, American Cancer Society, Ovarian Cancer Research Alliance, and private organizations. The awarded research grants focus on a variety of critical questions in gynecologic oncology, including overcoming therapy resistant ovarian cancer, innovative clinical trials, precision medicine against recurrent endometrial cancer, and the development of novel ovarian cancer therapies.
Faculty Profile: Saketh R. Guntupalli, MD
By Heather Aldrich, PhD
 Dr. Saketh Guntupalli was attracted to the field of oncology largely due to the data-driven focus of cancer care. He attended Johns Hopkins University for his undergraduate degree, then attended the University of Texas at Houston for his medical degree. After medical school, Dr. Guntupalli completed his residency in obstetrics and gynecology at Baylor College of Medicine, then pursued a fellowship in gynecology oncology and advanced pelvic surgery at Washington University in St. Louis. His passion for data-driven cancer care has lead Dr. Guntupalli to be a national and international expert in women’s cancer as well as the molecular mechanisms of cancer.
Dr. Saketh Guntupalli was attracted to the field of oncology largely due to the data-driven focus of cancer care. He attended Johns Hopkins University for his undergraduate degree, then attended the University of Texas at Houston for his medical degree. After medical school, Dr. Guntupalli completed his residency in obstetrics and gynecology at Baylor College of Medicine, then pursued a fellowship in gynecology oncology and advanced pelvic surgery at Washington University in St. Louis. His passion for data-driven cancer care has lead Dr. Guntupalli to be a national and international expert in women’s cancer as well as the molecular mechanisms of cancer.
For the last 10 years, Dr. Guntupalli has been providing research and clinical expertise at the University of Colorado Anschutz Medical Campus. Dr. Guntupalli has been instrumental in starting the Ovarian Cancer Center and is passionate about the team of researchers and clinicians he works with to provide patients with personalized care. The collaborative team involved with the Ovarian Cancer Center is dedicated to advancing the field of ovarian cancer by looking at markers to predict and treat cancer.
Dr. Guntupalli has continued to pursue data-driven cancer care by helping grow one of the largest groups in the world focused on providing the best care to patients with ovarian cancer. Dr. Guntupalli has held a variety of leadership roles for his work in gynecology oncology, written many clinical publications, and authored a New York Times reviewed book. One of Dr. Guntupalli’s favorite activities outside of work is hiking in the summer – while Colorado is green and peaceful.